How to deal with Critically Ill patients - 101 (The Bare Basics)
Getting assigned to man the acute beds can be daunting. There are so many issues to tackle and many things can go south in a moment's notice. New patients will need to have their direction of care established swiftly as decisions have to be made to dialyse (all-out approach) or buy time (wait it out).
More often than not, medical wards aren't suitable for critically ill patients as they require intensive monitoring by the clock. High Dependency Units (HDUs) or Intensive Care Unit (ICU) are designed to handle patients nearing the edge of death or require continuous monitoring of their physiological states. The goal is to buy more time so that the primary team can figure out and treat the underlying cause, hence suitable for patients with a reversible cause in mind.
Not all patients who present show signs of impending deterioration and patients with potentially severe conditions could deteriorate in the ward despite proper measures taken in the Emergency Room (ER) or acute bay. If you ever get stuck managing the acute beds, here are some tips I learnt that help me prevent catastrophic events from happening.
1. Proper history and physical examination
Everybody should start from here. Nobody can run away from fundamentals. A patient's presenting complain can bring you a long way to narrowing down differentials, instead of shooting at everything under your guesswork with investigations. A simple "chest pain" has already narrowed the problem to the thoracic region or upper abdomen. You should build up your case base on the signs & symptoms (evidence).
2. FAST HUG BID
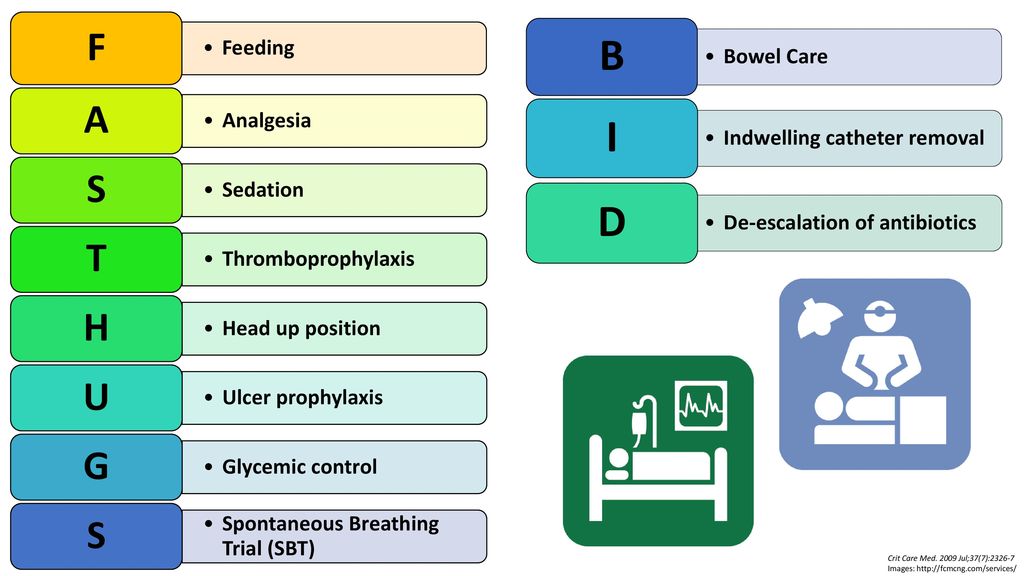
This may be relevant in the ICU setting, but if you "FASTHUG" all your acute beds, you can rest easy at night. (That is how solid this mnemonic is!)
Once you have narrowed down the diagnosis (with your history, physical examination, investigations), you can buy time for your treatment to work / definitive investigations to come back by stabilising the patient and prevent complications.
Fluids / Feeding - Critically ill patients require adequate nutrition for recovery. They will also need hydration for cellular function. An estimated daily insensible loss is ~ 500cc. Do not overload patients.
Analgesia - Surgical conditions require adequate pain relief, especially in those with pre-existing Ischaemic Heart Diseases (IHD). Pain increases the workload of the heart, thereby increasing myocardial oxygen demand, causing a mismatch in oxygen delivery to an area supplied by a stenosed vessel of the heart. Analgesia is also important for early mobilisation and recovery. Aim for pain score less than equal of 4.
Sedation - Cerebral protection is important in certain conditions, ie ROSC patients, Status Epilepticus patients, post-operative neurosurgical patients. It also reduces cerebral ischaemia, prevents secondary brain injury.
Thromboprophylaxis - Always review if the patient has any contraindication for anti-coagulants. The best example would be among postpartum patients. Before prescribing any drugs, always ensure lifestyle changes are in place. Adequate hydration, ambulation, physiotherapy, TED stockings are all important measures with minimal side effects. They should be considered first.
Head up 30 degrees - This improves venous return from the brain to the heart, reducing intracranial pressure. It also reduces abdominal splinting of the diaphragm, preventing lung collapse.
Ulcer prophylaxis - Any standard Proton Pump Inhibitor (PPI) will do the trick. This is to prevent stress ulcer formation. The simple reason would be a reduction in blood flow (ischaemia) to the stomach, thinning the alkaline protective mucous membrane of the inner wall lining. Increase in gastric acid production further damages the gastric wall, causing ulcer formation. The last thing you want happening in a critical patient is an upper gastrointestinal bleed. Of course, side effects are hypomagnesaemia, etc. As long as feeding is ongoing and the patient is young, I wouldn't be too concerned but still cautious.
Glucose - Blood glucose monitoring and optimisation are vital, especially in diabetics. You would typically accept a higher range in critically ill patients (not more than 12mmol/L). Treat hyper/hypoglycaemia accordingly.
Spontaneous Breathing Trials (SBT) - There are proper guidelines on how to wean a patient. I typically let the anaesthetists handle this as it is their expertise. (They also own the ventilators)
Bowel / Bladder - Believe it or not, constipation is one of the causes of delirium. It also decompensates liver failure patients. Ensuring your patient passes motion daily is essential. Urine output is an indicator of acute kidney injury and hydration status.
Infection - Secondary infections & sepsis is catastrophic, especially with hospital-acquired bugs. The sepsis 6 bundle must be applied with proper antibiotic stewardship. This should be anticipated in patients with prolonged stay. Always watch out for thrombophlebitis, urinary infections or femoral catheter infections! Change all tubings every 2 weeks!
De-escalation - After you have optimised everything from the above, you should consider aspects in which you can de-escalate your support. Antibiotics can be oralised. Urinary catheters can be removed if not needed. Fluids should be cut down according to the R.O.S.E concept.
3. Adress the issue
Now that you have stabilised the patient, you should discuss with your superiors on how to tackle the main issue. You should not delay time in referrals or starting important drugs once the diagnosis has been established. Diagnostic investigations should be expedited. Multidisciplinary teams (MDT) should be formed to tackle the matter at hand and address any existing complications.
4. Communication & Documentation
Patients and family members should be updated on the patient's latest condition and efforts the MDT is taking to address the issue. The pathophysiology should be explained in layman terms so that family members understand the nature of the disease. This will ease the discussion on the ceiling of care. Concise documentation should be done regarding the patient's progress and discussion for future reference.



Comments
Post a Comment